
I breathe a sigh of relief today as I sit drain-tube-free, surgery complete, and finally on what feels like a “break” from treatments from now until after birth. Still bandaged up and sore but feeling a version of finished-for-now… the relief I think everyone expected me to feel after my final chemotherapy treatment but I didn’t, knowing I had one more big pre-birth hurdle to get through before I could really exhale.
The last month has not been an easy one, recovery from the final chemotherapy treatment being the hardest one yet, the most exhausting, the longest to recover from, and worst of all, the most mentally challenging. I had a good ten days after my last chemo session of feeling so low I was googling depression-as-a-chemotherapy-side-effect… finding a good amount of papers on a link of depression as a physiological *side effect of the drugs* I was on made me feel reassured and able to tell myself “this feeling will pass” as I waited for my body to recover from the past 6 rounds of chemotherapy treatment. And it DID pass, the cloud lifting slowly and my mood, energy and colour-in-my-face coming back gradually and eventually, but at a decidedly slower pace than previous treatments.
On December 19th, the same date my good friend’s son had had heart surgery as a baby 12 years ago, my own long and warily anticipated surgery day arrived. This felt significant because I’d recently been given a handmade baby quilt hospital volunteers had made for little baby Nash after his own surgery to come home in all those years ago, and I felt like I had this amazing kid’s strength with me and my baby for the ride on the anniversary of his own surgery. My scheduled surgery came the day after confirmation of a serious health condition in another family member, and I have to say there has been a real feeling of “and the hits just keep on comin'” around here so all the symbols of strength and love were welcomed.

Surgery day was a long day, and I tear up thinking about how much better it was made by my mom arriving to be at home to care for our dog and cook for and take care of us, AND by my friend and midwife being by my side for every moment of the day. Andrea, Gary and I started off with a pre-surgery procedure at one hospital in the morning, made a quick pit-stop for a reflexology massage to give our bodies / my body some gentle love and care on a day of invasive procedures and to keep my pregnant mind off the fact that I hadn’t been able to eat since the night before and was already starving, and then headed to another hospital for the surgery.
I was admitted. Blue hospital tag complete with a scanable QR code snapped around my wrist. Ushered into a waiting room with airport-like screens on the wall with “patient status” updates associated with confidential patient numbers scrolling by on the screens like flight-statuses. Arrived. Pre-Assessment. Surgery Started. Surgery Stopped. Efficient and streamlined and dehumanizing at once.
In the pre-operation area. Waiting for my surgeon and anesthesiologist to come and speak to me. Clothes off, blue patient gown on. Placenta necklace handed over to Andrea to wear during surgery. Bracing myself because despite having convinced the anesthesiologist in my original consultation way back in July to do nerve blocks for me instead of putting me under General Anesthetic, the norm for this type of surgery, I KNEW I was going to have to advocate for it again. They had forgotten to book my pre-op consult to speak again with anesthesia, even though I had called several times, explained why it was important and that I was concerned something would be overlooked since I’d requested something non-standard, but I kept getting brushed off and falsely reassured over and over again that of course I would get my appointment and of course nothing about the plan had changed.
My surgeon came to speak to me first. I expressed my growing concern that I still hadn’t spoken to anesthesia, could tell by her response that it was NOT expected that I’d be staying awake as requested for the surgery, and she told me she’d get anesthesia to come speak to me right away. While waiting, my midwife looked at me lying down on my back in the hospital stretcher, in my patient gown and looking – and feeling – vulnerable. She put her shoulders back and said, “Okay Jessica. Sit up now” in the strong voice of hers that reminds me of my own strength. I knew right away what she was saying: sit up. Make yourself a strong equal here, not a passive patient lying down and looking up at the fully clothed “authority figures” above you. Find your confidence.
The anesthesiologist came and and, sure enough, the idea of keeping me awake was all news to him and he tried somewhat to talk me out of it. The nerve blocks and local anesthetic might not be sufficient, they don’t want me to suffer, this surgery is really invasive. He got the colleague who would have to be the one to do the nerve blocks to come and talk to me as well. None of the info they were giving me was new – I’d had all of the pro-and-con convos with the original anesthesiologist, done research myself, and had long ago decided that staying awake and only going under GA if the alternative method failed was the route that felt best for me personally, but sitting there undressed, moments before being taken into the OR, feeling at their mercy because delaying surgery if they refused to do anything other than GA felt not possible (I’m already so pregnant!), made me feel like so many pregnant people feel when providers attempt to get them to change their mind about what they want mid – birth. Bubblings of self doubt and a wavering confidence about the choice I had already made, was well informed on, and nothing had changed around my circumstances about except needing to re-decide and re-insist upon it being what I wanted. I’m all-too familiar with this scenario with clients and the impact it has on them.
“Why don’t you want the GA?” They asked. Because I’m pregnant. Because although GA in pregnancy has been found to be reasonably low-risk, NOT being under GA is better. Because having quite intense surgery while pregnant and unconscious simply felt way too vulnerable – handing my body and baby over completely to other people’s judgement while I was unconscious was not something I was personally okay with. I wanted to be a part of it, I wanted to be able to feel my baby move and be connected to the baby during the surgery, and if anything unexpected arose during surgery, I wanted to be INVOLVED in any decisions, not to wake up to being told about anything that might have happened while I was unconscious. Truth be told, my biggest fear was waking up with the baby outside of my body, even though I knew there was extremely little chance of that happening. While I believe the surgery itself was also quite low-risk for the pregnancy, I wanted to keep it AS low risk as possible and be as a part of it as possible, though certainly other people would have their own reasons for preferring GA for surgery, pregnant or not. They said they understood my reasoning and offered Gary and I a few minutes to talk so I could (re-)decide.
The doubt had wiggled its way in there, though. Having to re-go over the “what ifs” of “what if it doesn’t work” at the last minute, even though I’d factored that possibility in when I’d originally made the decision made me doubt myself and I was wavering. Gary reminded me that he supported me no matter what, and also that nothing had changed, we had learned nothing new about the options, and reminded me of what he’d heard me say for months that I wanted – that I really did NOT want to be put out for the surgery unless absolutely necessary. Thank goodness he’s ALSO had years of training in how to support people navigating the medical system through endless stories of my work in birth. His confidence in me gave me a helpful extra nudge of strength to call the anesthesia team back in and say firmly, “I want you to try”.
Time for the two nerve blocks to be administered. Sit up. Feet over the side the of the bed. Curl around a pillow and round out your back for the needles to go in. I caught my midwife’s eye and said, “Well, this is ironic, isn’t it?”, alluding to how reminiscent this was of how epidurals are administered during birth.
Next, wheeled on the stretcher into the OR, holding my pregnant belly, looking up at everyone in scrubs around me. Center of the room. Bright lights. Surgical drape placed in front of my face, a sea of indistinguishable masked faces peering over the screen to mutter instructions or introducing themselves to me, eerily familiar as so similar to the scene during cesarean births I’ve witnessed over the years. My legs started to shake, and my midwife put her hands on my shoulders and talked me into my body, helping me to breathe and relax into the surgical bed. “I’m okay I’m okay, I’m okay”, I whispered to myself. “I’m okay, I’m okay, I’m okay.” I focused on my pregnant belly and my squirming baby moving healthily inside my body. I pictured my Rose Namajunes poster on my bathroom wall, and heard in my head words Andrea had said to someone earlier in the day: “Jess is tough as nails”.

My surgeon was tuned in and connected to me the entire time through the 3 hour surgery, asking me if I was okay, adding local anesthetic as needed and noticing when I was lying about not being in any discomfort because “I can see your pulse go up.” The anesthesiologist added a small amount of analgesic through my IV when I needed it. At one point my surgeon noticed my breathing change and checked in with me – I told her it was the sound of what she was doing that was giving me anxiety and she asked someone to find some speakers to play music for me.
I focused on the lyrics from a recent doula training playlist of mine, focused on Andrea’s hands on my head, focused on my breath (in and out, deep and slow), and focused on the baby moving in my body. I told myself I was safe, and tried to visualize myself somewhere peaceful and serene, or at some kind of weird alternative medicine spa to keep my mind from picturing what the surgeon was actually doing. “I come into the peace of wild things…”
Eventually it was over, the surgeon feeling confident she’d gotten out everything she‘d needed to (though pathology results are yet to come), and not surprised that I wanted to go home instead of staying overnight. Andrea stayed with me for my couple of hours in recovery, and until after Gary arrived back from home to meet me. After a lovely check-in from a nurse friend who works in the recovery room (a much welcomed familiar face), we headed back home. To my own bed, to a home-made nourishing meal prepared by my mom, and to an environment that felt much more healing and restful than a germy and disruptive hospital room would have been.
When I saw the surgeon the next day for a quick follow-up, I said to her, “I know most people wouldn’t want to have been awake for that and understand why, but just so you know, it was definitely the right choice for me. I’m really glad I did it that way and am really grateful to have had that option.” I wanted her to know I didn’t regret my choice, it was 100% the right thing for me. She chuckled somewhat and said, “Jessica, not MOST people. Like 99.99% of people.” At some point she said to me, “Well, you sure are brave. You are going to have no problem giving birth.” Which felt like an amusingly doctor-like way to be encouraging about childbirth. One could argue brave, or perhaps a sign of being too afraid of giving control of certain things over to others (my teacher recently teased me “you are severely crippled in the area of trust!”), but either way! I like that I’ve been able to embrace having trust in myself more than anything.
For the last 10 days, I have been recovering at home, stitched and bandaged up, a drain tube coming out of my armpit to prevent fluid build up in my healing wound areas, being fed and cared for by my mom. Dad joined us for a few days for a quiet and restful Christmas before they both went home yesterday. The drain was removed today, and the wounds for both the axillary node dissection (removal of all lymph nodes in the affected arm) and lumpectomy (for those dying to pry as to “what kind of surgery did you have?) seem to be healing well, though my arm has rather limited mobility and discomfort and nerve pain that I will be doing physiotherapy for.

Birth is next on the list to look forward to in a few months, but be patient while this baby continues to grow and gain strength to be ready to be born and resist the urge to guess when it will happen. The baby and I both need some recovery time! Radiation will come sometime postpartum, which will be a whole other layer of daily treatments to add to the typical postpartum period, but that’s a bridge to cross when I get there and not something to think about for now.
While I’m not interested in unsolicited advice or suggestions, I AM opening the door to messages repeating back to me phrased or encouraging words you may have heard me during or about birth or postpartum that you found particularly helpful or inspiring or encouraging for yourself if you were my client or that has struck a cord with you as a birth worker or friend. I’m not the best at taking advice but I can’t argue with my own advice being given back to me, so THAT I am open to hearing ;). You can email or text me if you have my number.
Still not looking for any other place advice or suggestions and still not taking questions about why I made certain choices or about details about future plans beyond what I am openly choosing to share here, and still not interested in getting specific about when I’m “due” beyond end-of-winter-or-early-spring. Try to find some magic in the mystery, like I have.
Happy New Year everyone!! This year has been a big one, to say the least! Thanks to everyone for all the love and care they have given us all year in various ways. It’s made such a difference.
I have loved the stars too fondly to be fearful of the night.” ~Sarah Williams
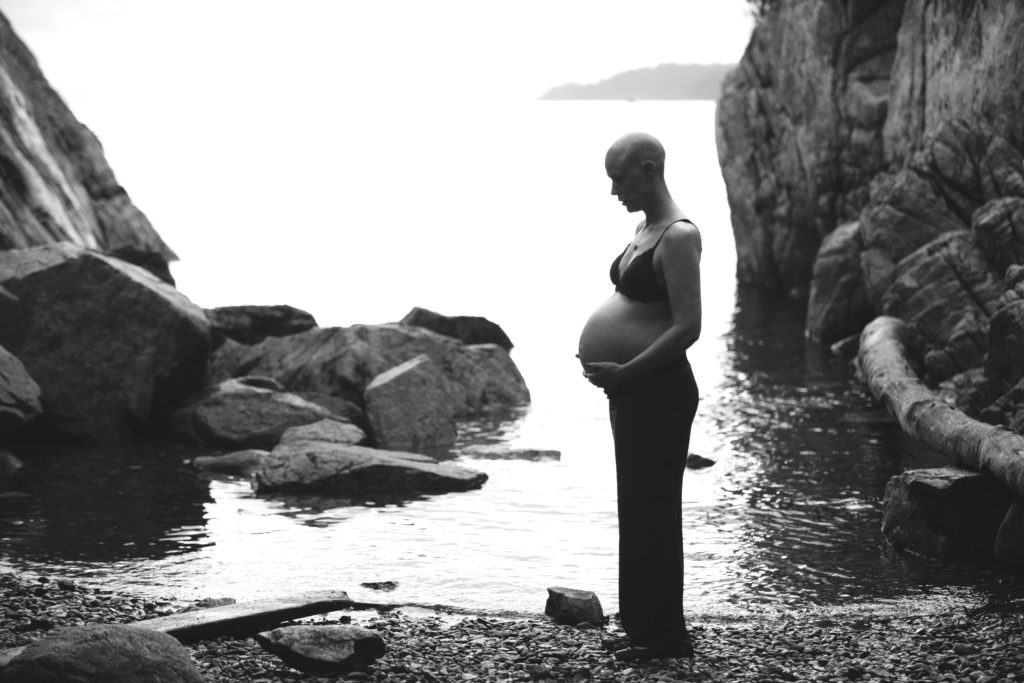
Photos: Kristie Robin, kristierobin.com
___________________________________
If you missed previous posts, you can find them here.
You can still send folks to my website if they are looking for birth support, prenatal classes, or doula trainings while I’m on leave! Talia and Meena are holding down the fort here, and Gloria will be primary instructor for Wise Woman Way of Birth next year while I’m off. Don’t hesitate to keep reaching out to us!
You can also follow me on instagram @jessicaaustinchildbirth




